Data and measurement are key components to improvement. As I wrote about in my previous two blog posts, a Tokyo hospital that I visited twice last month (both for a short site visit and discussion with the President, and later to sit in on their monthly Quality Committee meeting) is focused on quality data and continuous improvement.
I was aware of this hospital’s focus on data-driven improvement because I had heard a presentation the hospital president had made at the Conference for Healthcare that I attended in October. However, I hadn’t realized quite what a leader in Japan this hospital is in data transparency until I met with the President on my first visit.
During our meeting, he gave me two copies of an annual “Quality Indicators” publication that the hospital produces – one from 2015 (in Japanese) and one from 2013 (that had been translated into English). Since that initial meeting, I’ve had a chance to read much of the English edition and talk further with some of the Quality leaders at the hospital.
In this post I’ve included some of my reflections and take aways from the Quality Indicators publications.
Japanese leader in data transparency

This Tokyo hospital started to measure quality indicators (QI) in 2005, upon the appointment of the President, and began publicly sharing its data via publication a few years after that. I don’t know how many Japanese hospitals share their data publicly, but I doubt many publish annual reports of the extent that that this hospital does.
When I first started working in hospital quality improvement ten years ago, the topic of data transparency was an emerging one. The hospital that I worked for, Lucile Packard Children’s Hospital (now called Stanford Children’s Hospital) in Palo Alto was one of the first children’s hospitals in the United States to publish its quality data on the web.
Annual Quality Indicators Publications
This hospital’s Quality Indicator reports not only present the final data, but describe the performance and what was done over the course of the year to contribute to the results. Similar to my experience in observing the Quality Committee meeting, the presentation of the data is clear, though often in less detail than what was presented at the Committee.
Quality Indicators
There are 71 QI included in the 2013 English edition and 73 in the 2015 edition, ranging from clinical indicators (both process indicators such as “beta-blocker given at arrival” and outcomes indicators such as “mortality rate”) to patient satisfaction indicators to operational indicators (e.g. length of stay, employee non-smoking rate, nursing educational background, etc.).
Additionally, the book describes how the QI Committee identifies “approximately 10 indicators with priority need for improvement” that are set targets that must be achieved within a year and are monitored regularly at the QI Committee meeting.
Don’t just measure, but IMPROVE
The subheading of the 2013 publication is “Measuring and Improving Quality of Medical Care” (bold emphasis in original). This reflects an important belief at the hospital that it’s not just data that is important, but rather how the organization uses data to drive improvement.
From data to kaizen
Since the inception of the QI reporting in 2005, the organization notes in the 2013 edition that is has “shifted from simply measuring and reporting QI to conducting QI improvement programs”. The President had shared with me that he is happy that Quality and QI are common language now in the hospital.
Their next goal is to continue to improve and build upon this use of data through more direct frontline engagement in kaizen. For example, the hospital has recently put up QI visibility boards in each unit that the managers use to discuss local quality improvement opportunities with the frontline.
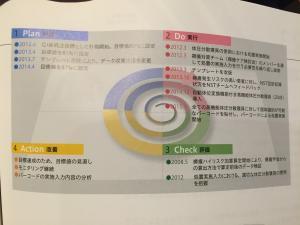
PDCA
As the President shared with me, and as evident at the Quality Committee meeting, this hospital uses PDCA (plan-do-check-act) as the foundation for their improvement efforts.
In the 2015 publication, as compared to the 2013 publication, the hospital has moved to showing the PDCA format that they used in the Quality Committee for reporting out the high-level improvement plan.
Measure yourself and seek to improve
This hospital places more emphasis on measuring themselves and seeking continuous improvement.
“The author [the hospital President] believes that the primary objective of measuring and publishing QI [quality indicators] should not be a cross-sectional comparison across multiple medical establishments but the longitudinal improvement of the quality of examination and treatment in individual establishments.”
In many hospitals and healthcare systems in which I’ve worked, leaders invariably want to see comparisons to “best practice”. I get concerned when I hear this – not because it isn’t good to know what other organizations are doing or to learn from their successes or challenges – but it can limit us in thinking about what more might be achieved.
Instead, like this hospital’s President, I am a proponent of organizations comparing themselves to their OWN data and to seek continuous improvement towards attaining perfection (even if perfection isn’t seemingly attainable).
This is one reason why Toyota always seeks *zero* defects and why I believe we should always seek zero defects in healthcare as well. This can be a contentious topic among healthcare leaders, but is one that I always put forward.
Upcoming discussions about healthcare improvement and quality
The Medical Director of Quality and one of the Quality Managers have agreed to meet with me in a few weeks for us to talk further about the quality improvement approach at this hospital, and for me to share some of my experiences in applying “industry” / Lean tools and processes in healthcare.
I have also made an appointment to visit another Tokyo hospital and talk with their President later this month about their Total Quality Management (TQM) approach to improvement.
I’m eager to learn more from both of these organizations and look forward to sharing whatever information that I learn that they are willing for me to write about.
What questions do you have?
Some of you have sent me questions that you are interested in learning about, many of which were on my mind as well.
Questions include:
- How is patient input collected and used for improvement?
- What is their methodology(ies) for improvement?
- How do they implement PDCA?
- QI Committee – who attends and why? What do they get out of the meeting?
If you have additional questions, please let me know via the comments section below and I will include them in my list.